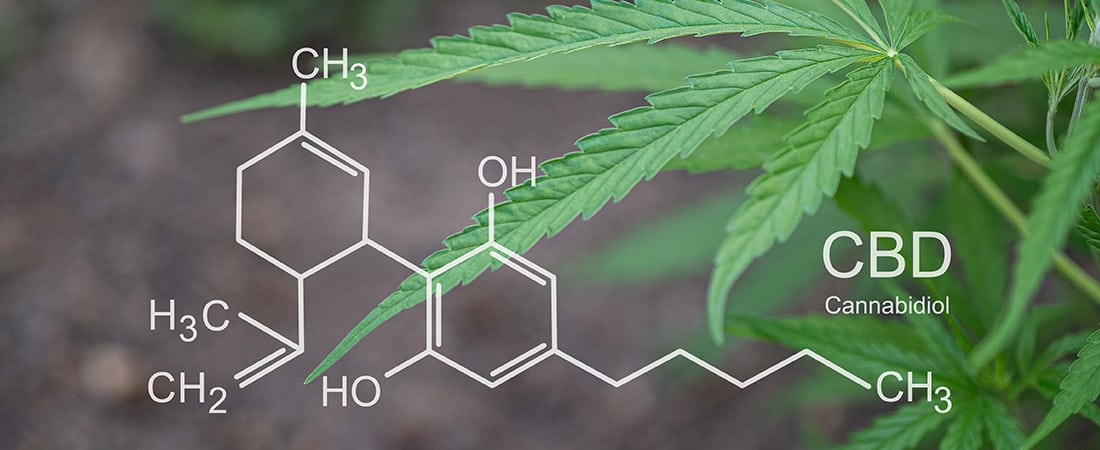
Cannabidiol (CBD) is the second most common phytocannabinoid found in cannabis plants after tetrahydrocannabinol (THC). In contrast to THC, CBD has not been shown to have a psychoactive effect. Due to its impact on several neurotransmitter systems, it has been tested for the treatment of many physical and psychiatric diseases due to its neuroprotective and anti-inflammatory effects. In this article, the characteristics of the CBD and its role in various psychiatric diseases are briefly reviewed. All our Products in our CBD Shop are not for medical purpose.
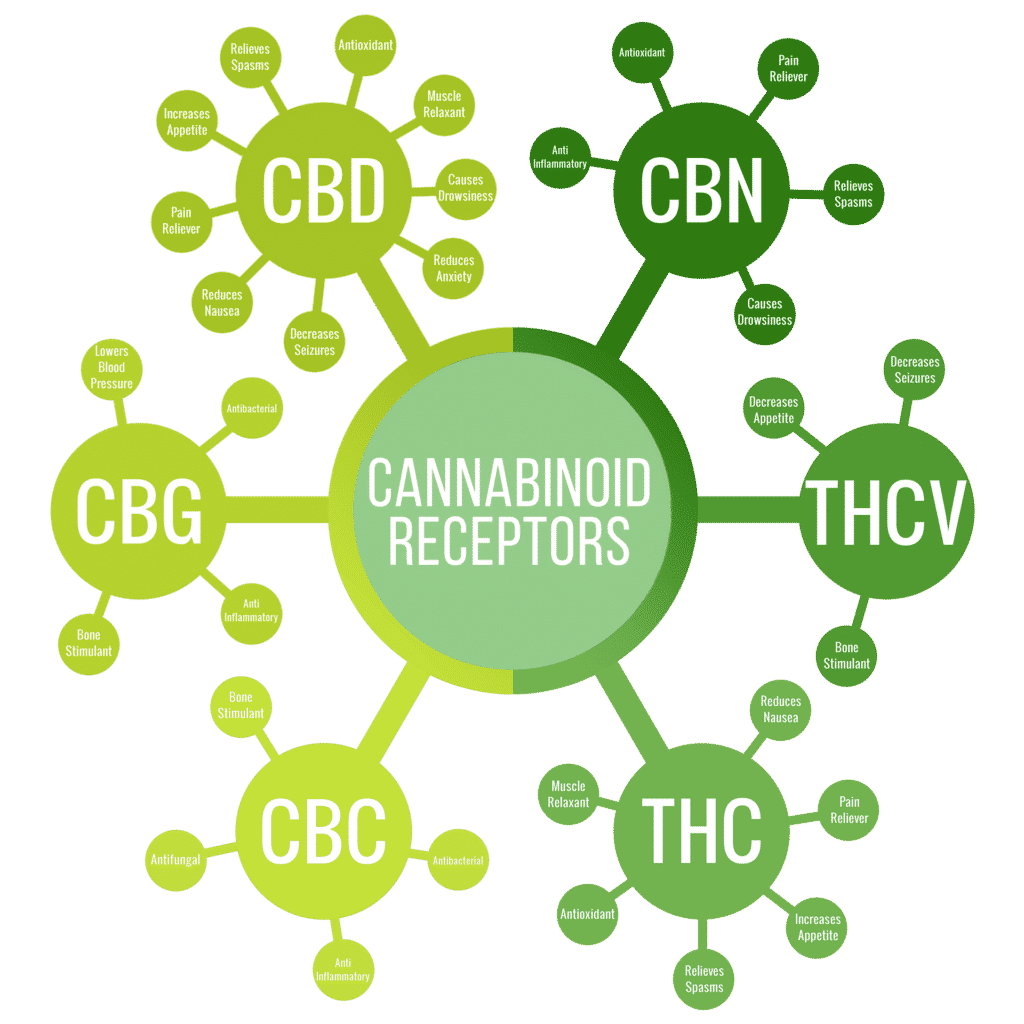
Cannabidiol (CBD) is a phytocannabinoid that is extracted from the Cannabis sativa plant like tetrahydrocannabinol (THC), but unlike the latter, it does not exhibit psychoactive effects. In contrast to THC, CBD does not trigger the reward system; however, it does act on the opioid, serotonin and cannabinoid receptor systems. Hence, it is considered promising for the treatment of drug addiction. In this context, it acts as a non-competitive antagonist of the CB1 receptor inside the cannabinoid system (1).
Nevertheless, it has been observed that CBD does not specifically impact the CB1 receptor. Most studies stated that it has no effect on the CB1 receptor at all, while a few studies showed mild agonistic or weak antagonistic effects. CBD also has a low affinity for another cannabinoid receptor, the CB2 receptor (2). CBD can be transformed to THC in some animal species and in laboratory situations, but this transformation does not take place in the human body (2,3).
Due to its effect on several receptors, the impact of cannabidiol is being studied in many physical or psychiatric disorders. Clinical trials for the treatment of epilepsy are underway and positive results have been published. In some pre-clinical studies, although not primarily in epilepsy, CBD has been reported to have neuroprotective, anxiolytic, antipsychotic, analgesic, anti-inflammatory, anti-asthmatic and antitumoral properties (2). The medical use of CBD has also been evaluated in disorders of substance use. A number of preclinical studies have shown that CBD may have a therapeutic impact on dependence on opioids, cocaine and psychostimulants. Some studies have also provided data suggesting that CBD may be effective in cannabis and tobacco dependence in humans (4).
The use of substances leads to an imbalance in the mesolimbic circulation. CBD mitigates this dysregulation when dosed regularly. Due to this property, CBD has been considered beneficial in cases of substance use disorders. It is believed that its effectiveness may depend on the dosing and whether it is given before or in combination with the substance used (1). It is also assumed that CBD reduces the rewarding effect of substance use through 5HT1A receptor agonism, which effectively decreased stress and anxiety in the mesolimbic system. This proposal is based on selective serotonin recovery inhibitors and other antidepressants that reduce substance use by relieving mood symptoms. CBD has been suggested to have a therapeutic impact on substance use disorders by reducing stress, anxiety and depressive symptoms (1).
CBD has adverse effects such as sleepiness, digestive disturbances and fatigue, and it can also cause drug interactions and cause an increase in liver function tests. Suicidal thoughts, which are uncommon with other anticonvulsants, can also occur when using CBD. Therefore, its influence on suicidal thoughts must be investigated (5).
The dependence potential of THC and CBD was compared in mice, in which tolerance to THC but not to CBD increased. Furthermore, there are no clinical studies showing that CBD has a potential for addiction or abuse (2). One study showed that the potential for abuse of CBD is placebo-like compared to cannabis in humans (6). Polydrug users have shown that the potential for misuse of a therapeutic dose of CBD is low. However, high doses of CBD have been shown to have greater perceived effects compared to placebo, but these are significantly lower than those observed with alprazolam and dronabinol (7).
Alcohol and Cannabidiol
Alcohol has been shown to cause damage to the frontal and temporal lobes and the hippocampus, particularly through the induction of neuroinflammatory mediators and/or oxidative stress. It is known that these brain areas are related with problem solving, attention, information processing, learning and memory (8). Since CBD has neuroprotective impacts that prevent oxidative damage, it has been proposed as a therapy form against cognitive disorders caused by alcohol. These effects of CBD are thought to be mediated by the 5HT1A or CB2 receptors (8). Although the results are based on pre-clinical studies, they have been reported to support the potential therapeutic benefit of CBD in alcohol-related disorders, particularly in the areas of neurodegeneration, hepatotoxicity, cognition and risk of recurrence (8). In addition, CBD may have a therapeutic effect in alcoholic liver diseases characterized by inflammation, oxidative stress and steatosis (9).
A study in male mice using a strain that willingly drank ethanol showed, that a supplementation with CBD reduced the reinforcing properties, motivation and ethanol relapse. Based on these results, the authors proposed that CBD could be useful in the treatment of alcohol consumption disorders (10). In another animal study, simultaneous administration of CBD and naltrexone was shown to be more effective than either CBD or naltrexone alone in lowering ethanol consumption and drinking motivation. These effects have been found to be at least partially mediated by 5-HT1A receptors (11). However, it should be pointed out that the number of these studies is small and additional clinical research is required.
Cannabis and Cannabidiol
The effectiveness of the agonist therapy on cannabis dependence is limited (12). Consequently, alternatives to pure agonist treatment are also being examined. It has been shown that a treatment with CBD reduces behavioral disorders associated with cannabinoid abuse in mice, indicating that it supports CBD utilization in cannabis dependence (13). In a study with 20 cannabis consumers who had consumed cannabis for an average of 5.5 years, it was found that CBD has positive effects on attention control and psychological symptoms caused by cannabis dependence. Furthermore, the study revealed that CBD had more benefits among dependent cannabis consumers than among non-dependent consumers. (14). In another case study, a cannabis addict with bipolar disorder was supplemented with CBD; cannabis consumption was stopped, and sleep patterns improved (15). In another case report, CBD has been shown to be beneficial in the treatment of cannabis withdrawal symptoms (16). Nevertheless, it was reported that CBD may have the ability to reduce euphoria linked with cannabis use, even if it does not directly reduce cannabis use (14). Lastly, no positive effects of oral CBD on the enhancing, physiological or positive subjective qualities of cannabis have been observed (17).
Opioids and Cannabidiol
Most research on the impact of CBD on opioid use disorders used animal experiments. Recent research has shown that CBD blocks the rewarding effects of morphine (18). CBD has also been found to be effective in heroin studies on rats. In a study that investigated the effects of CBD on self-administration of heroin and drug-seeking behavior in an animal experiment, it was proposed that CBD could be a potential treatment for heroin addiction and relapse (19). In this study it was further revealed that heroin self-administration was not changed by CBD dosing, but cues-induced heroin search was clearly suppressed. Even when heroin was given during active heroin use, the ability of CBD to prevent relapse was demonstrated even in the weeks following the most recent treatment. On the basis of these findings, the authors of the study presumed that CBD might influence heroin addiction even after a possible relapse after a period of deprivation (19).
Cocaine, Psychostimulants and Cannabidiol
The findings concerning the effectiveness of CBD with the application of stimulants are controversial (1). There are studies showing that intensive treatment with CBD does not block the rewarding effect of cocaine (18), does not reduce self-administration of cocaine, and does not reduce cue-induced cocaine use in rats: Intensive CBD treatment had a minimal effect on cocaine uptake and relapse in a rat model (20). Despite CBD did not reduce drug-induced rehabilitation, it did reduce voluntary cocaine use (21). Because CBD has been shown to be effective in preventing methamphetamine-induced “Conditional Place Preference” (CPP) in rats even under stress, it has been suggested that it could be used to reduce the risk of relapse (22). Varying results have also been found in studies on the recurrence of psychostimulants and cocaine. CBD is able to mitigate reconsolidation of CPP for cocaine in mice (23) and effectively lower stress-induced cocaine recovery (24). In another study, no effect of CBD on drug-related rehabilitation after extermination was found (21). The differences between the results obtained may vary on the dose (25). CBD has been found to lower the motivation to seek and use methamphetamine and may therefore be a viable pharmacotherapy for methamphetamine dependence (25). The effect reported in this study was observed at a dose of 80 mg/kg CBD, but not at 40 mg/kg or 20 mg/kg. In another study, CBD has been stated to be useful by mitigating the acute rewarding effects of cocaine through a mechanism associated with DA (26).
Tobacco and Cannabidiol
Since the endocannabinoid system is believed to play a role in nicotine addiction, the efficacy of CBD in this regard has been examined through several studies on dependent smokers. In one of these studies, 24 smokers were divided into two groups that received CBD (n=12) or placebo (n=12) during a one-week treatment. There was no variation in the number of cigarettes smoked in the placebo group, while those who received CBD lowered the number of cigarettes smoked during treatment by about 40%. The results also indicated some consistency in the follow-up. These provisional data indicate that CBD is a potential therapy method for nicotine dependence (27). In another study involving 30 subjects, a single dose of CBD reduced the convenience and visibility of cigarette cues compared to placebo after night-time abstinence in dependent smokers. However, CBD had no effect on tobacco craving or withdrawal (28).
Psychosis and Cannabidiol
There are pre-clinical (29,30) and ongoing clinical studies on the antipsychotic effectiveness of CBD (31). First, a single case report has shown that CBD leads to improvement in a patient with treatment-resistant schizophrenia (32). A four-week randomized, double-blind clinical study was conducted on 42 schizophrenia patients comparing “Amisulpride”, a very potent second-generation antipsychotic, with CBD. The patients received either CBD (600-800 mg/day) or Amisulpride (600-800 mg/day). Both drugs showed a significant improvement of both positive and negative symptoms of a psychosis. The efficacy of cannabidiol was as good as that of Amisulpride. In addition, the side effect profile of CBD was superior to that of Amisulprid (33). CBD did not cause prolactin elevation, weight gain or extrapyramidal symptoms observed with Amisulpride. A reduction in psychotic symptoms associated with elevated serum anandamide levels in patients receiving CBD treatment suggested that inhibition of anandamide deactivation may be contributing to the antipsychotic impacts of CBD (33). An fMRI study indicated that CBD could potentially normalize changes in the function of the parahippocampus, striatus and midbrain, which are important in the pathophysiology of psychosis, leading to therapeutical effects of CBD on psychotic symptoms (34).
Anxiety and Cannabidiol
There is currently research being conducted on the effect of the CBD on anxiety (35). It has also been stated that CBD has been shown to prevent delta-9-THC-induced anxiety. This effect may be due to marijuana-like effects and other subjective changes caused by delta-9-THC, as no changes were found in pulse measurements (36). The anxiolytic impact of CBD on anxiety caused by a simulated public speaking test was proven in a clinical study. The results suggest that CBD has anxiolytic effects on volunteers exposed to stress (37). In a single-photon emission computed tomography (SPECT) study, CBD was shown to significantly reduce subjective anxiety, while placebo did not cause noticeable changes. These findings indicate that CBD can have anxiolytic qualities and that an effect on limbic and paralimbic brain areas mediates such effects (38). Using the same neuroimaging method, the efficacy of CBD and placebo was compared on 10 subjects with social anxiety disorder and it was shown that CBD reduces anxiety in this condition. This result was related to the impact of CBD on limbic and paralimbic brain regions (39). CBD was found to enhance the elimination of anxiety memories in 48 healthy volunteers, suggesting that it may be a useful addition to erasure-based therapies for anxiety disorders (40). CBD has been reported to have an anxiolytic effect by lowering physiological sleep with rapid eye movement (REM sleep) and non-REM sleep (NREM sleep) on normal rats. It has been implied that this is an essential finding for patients with post-traumatic stress disorder in whom sleep problems such as REM sleep disorders and insomnia are frequent (41). Based on the findings of preclinical and clinical studies, CBD can also be a potential therapy method for panic disorders (42).
Depression and Cannabidiol
In a study with mice, it was proposed that CBD increases both serotonergic and glutamatergic cortical signaling through a mechanism associated with the 5-HT1A receptor, making it useful as an antidepressant (43). Moreover, the findings obtained in an animal genetic model of depression indicate that CBD may be a potential treatment method for clinical depression and other conditions with significant anhedonia (44).
Alzheimer Disease and Cannabidiol
Given that Alzheimer’s disease (AD) is a neurological and psychiatric disease, it would be reasonable to consider the impact of CBD on this condition. Amyloid_β plaques and hyperphosphorylated taurine protein aggregate in the brains of AD patients characterized by neurodegeneration and high levels of oxidative stress and inflammation. As mentioned above, CBD has neuroprotective, antioxidant, and anti-inflammatory properties and therefore lowers amyloid_β production and tau hyperphosphorylation in vitro. CBD is believed to represent a new treatment option for AD as it has also been shown to be effective in vivo on this disease. The absence of psychoactive or cognitive inhibitory properties gives CBD an advantage in this regard (45).
Seizures and Cannabidiol
CBD has been approved by the FDA for two distinct forms of epilepsy, Lennox-Gastaut syndrome and Dravet syndrome (46). This is the first authorization for a medication derived from cannabis because CBD has not been approved so far for any other indication.
Conclusion
A review of the literature indicates that CBD may have a therapeutic effect in diseases such as substance use disorders, anxiety disorders, depression and Alzheimer’s disease, the last one being a neurodegenerative disease. These effects of CBD are transmitted by different receptor systems. However, most studies have used animal models rather than clinical trials. More clinical studies are needed for an effective use of CBD on humans. Nonetheless, the available data show that CBD will be a promising treatment method for various diseases and conditions in the future.
References
- Chye Y, Christensen E, Solowij N, Yucel M. The endocannabinoid system and cannabidiol’s promise for the treatment of substance use disorder. Front Psychiatry 2019; 10:63. [CrossRef]
- WHO (World Health Organization). Cannabidiol (CBD). 39th ECDD (Expert Committee on Drug Dependence) Agenda item 5.2. Geneva, 2017. https://www.who.int/medicines/access/ controlled-substances/5.2_CBD.pdf. Accessed [October 2019]
- Pisanti S, Malfitano AM, Ciaglia E, Lamberti A, Ranieri R, Cuomo G, Abate M, Faggiana G, Proto MC, Fiore D, Laezza C, Bifulco M. Cannabidiol: State of the art and new challenges for therapeutic applications. Pharmacol Ther 2017; 175:133-150.
- Prud’homme M, Cata R, Jutras-Aswad D. Cannabidiol as an intervention for addictive behaviors: a systematic review of the evidence. Subst Abuse 2015; 9:33-38. [CrossRef]
- White CM. A review of human studies assessing cannabidiol’s (CBD) therapeutic actions and potential. J Clin Pharmacol 2019; 59:923-934. [CrossRef]
- Babalonis S, Haney M, Malcolm RJ, Lofwall MR, Votaw VR, Sparenborg S, Walsh SL. Oral cannabidiol does not produce a signal for abuse liability in frequent marijuana smokers. Drug Alcohol Depend 2017; 172:9-13. [CrossRef]
- Schoedel KA, Szeto I, Setnik B, Sellers EM, Levy-Cooperman N, Mills C, Etges T, Sommerville K. Abuse potential assessment of cannabidiol (CBD) in recreational polydrug users: a randomized, double-blind, controlled trial. Epilepsy Behav 2018; 88:162-71. [CrossRef]
- Turna J, Syan SK, Frey BN, Rush B, Costello MJ, Weiss M, MacKillop J. Cannabidiol as a novel candidate alcohol use disorder pharmacotherapy: a systematic review. Alcohol Clin Exp Res 2019; 43:550-563. [CrossRef]
- Wang Y, Mukhopadhyay P, Cao Z, Wang H, Feng D, Hasko G, Mechoulam R, Gao B, Pacher P. Cannabidiol attenuates alcoholinduced liver steatosis, metabolic dysregulation, inflammation and neutrophil-mediated injury. Sci Rep 2017; 7:12064. [CrossRef]
- Viudez-Martinez A, Garcia-Gutierrez MS, Navarron CM, Morales-Calero MI, Navarrete F, Torres-Suarez AI, Manzanares J. Cannabidiol reduces ethanol consumption, motivation and relapse in mice. Addict Biol 2018; 23:154-164. [CrossRef] Evren et al. The good face of Cannabis sativa: cannabidiol 287
- Viudez-Martinez A, Garcia-Gutierrez MS, Fraguas-Sanchez AI, Torres-Suarez AI, Manzanares J. Effects of cannabidiol plus naltrexone on motivation and ethanol consumption. Br J Pharmacol 2018; 175:3369-3378. [CrossRef]
- Sabioni P, Le Foll B. Psychosocial and pharmacological interventions for the treatment of cannabis use disorder. F1000Res 2018; 7:173. [CrossRef]
- Garcia-Gutierrez MS, Navarrete F, Viudez-Martinez A, Gasparyan A, Caparros E, Manzanares J. Cannabidiol and Cannabis Use Disorder: In Montoya E, Weiss S (editors). Cannabis Use Disorders. Cham: Springer International Publishing, 2019, 31-42. [CrossRef]
- Solowij N, Broyd SJ, Beale C, Prick JA, Greenwood LM, van Hell H, Suo C, Galettis P, Pai N, Fu S, Croft RJ, Martin JH, Yucel M. Therapeutic effects of prolonged cannabidiol treatment on psychological symptoms and cognitive function in regular cannabis users: a pragmatic open-label clinical trial. Cannabis Cannabinoid Res 2018; 3:21-34. [CrossRef]
- Shannon S, Opila-Lehman J. Cannabidiol oil for decreasing addictive use of marijuana: a case report. Integr Med (Encinitas) 2015; 14:31-35.
- Crippa JA, Hallak JE, Machado-de-Sousa JP, Queiroz RH, Bergamaschi M, Chagas MH, Zuardi AW. Cannabidiol for the treatment of cannabis withdrawal syndrome: a case report. J Clin Pharm Ther 2013; 38:162-164. [CrossRef]
- Haney M, Malcolm RJ, Babalonis S, Nuzzo PA, Cooper ZD, Bedi G, Gray KM, McRae-Clark A, Lofwall MR, Sparenborg S, Walsh SL. Oral cannabidiol does not alter the subjective, reinforcing or cardiovascular effects of smoked cannabis. Neuropsychopharmacology 2016; 41:1974-1982. [CrossRef]
- Katsidoni V, Anagnostou I, Panagis G. Cannabidiol inhibits the reward-facilitating effect of morphine: involvement of 5-HT1A receptors in the dorsal raphe nucleus. Addict Biol 2013; 18:286- 296. [CrossRef]
- Ren Y, Whittard J, Higuera-Matas A, Morris C V, Hurd YL. Cannabidiol, a nonpsychotropic component of cannabis, inhibits cue-induced heroin seeking and normalizes discrete mesolimbic neuronal disturbances. J Neurosci 2009; 29:14764- 14769. [CrossRef]
- Mahmud A, Gallant S, Sedki F, D’Cunha T, Shalev U. Effects of an acute cannabidiol treatment on cocaine self-administration and cue-induced cocaine seeking in male rats. J Psychopharmacol 2017; 31:96-104. [CrossRef]
- Lujan MA, Castro-Zavala A, Alegre-Zurano L, Valverde O. Repeated Cannabidiol treatment reduces cocaine intake and modulates neural proliferation and CB1R expression in the mouse hippocampus. Neuropharmacology 2018; 143:163-175.
- Karimi-Haghighi S, Haghparast A. Cannabidiol inhibits priming-induced reinstatement of methamphetamine in REM sleep deprived rats. Prog Neuropsychopharmacol Biol Psychiatry 2018; 82:307-313. [CrossRef]
- de Carvalho CR, Takahashi RN. Cannabidiol disrupts the reconsolidation of contextual drug-associated memories in Wistar rats. Addict Biol 2017; 22:742-751. [CrossRef]
- Gonzalez-Cuevas G, Martin-Fardon R, Kerr TM, Stouffer DG, Parsons LH, Hammell DC, Banks SL, Stinchcomb AL, Weiss F. Unique treatment potential of cannabidiol for the prevention of relapse to drug use: preclinical proof of principle. Neuropsychopharmacology 2018; 43:2036-2045. [CrossRef]
- Hay GL, Baracz SJ, Everett NA, Roberts J, Costa PA, Arnold JC, McGregor IS, Cornish JL. Cannabidiol treatment reduces the motivation to self-administer methamphetamine and methamphetamine-primed relapse in rats. J Psychopharmacol 2018; 32:1369-1378. [CrossRef]
- Galaj E, Bi GH, Yang HJ, Xi ZX. Cannabidiol attenuates the rewarding effects of cocaine in rats by CB2, 5-TH1A and TRPV1 receptor mechanisms. Neuropharmacology 2019; 107740. [CrossRef]
- Morgan CJA, Das RK, Joye A, Curran HV, Kamboj SK. Cannabidiol reduces cigarette consumption in tobacco smokers: preliminary findings. Addict Behav 2013; 38:2433-2436. [CrossRef]
- Hindocha C, Freeman TP, Grabski M, Stroud JB, Crudgington H, Davies AC, Das RK, Lawn W, Morgan CJA, Curran HV. Cannabidiol reverses attentional bias to cigarette cues in a human experimental model of tobacco withdrawal. Addiction 2018; 113:1696-1705. [CrossRef]
- Osborne AL, Solowij N, Babic I, Lum JS, Newell KA, Huang X-F, Weston-Green K. Effect of cannabidiol on endocannabinoid, glutamatergic and GABAergic signalling markers in male offspring of a maternal immune activation (poly I:C) model relevant to schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 2019; 95:109666. [CrossRef]
- Jimenez Naranjo C, Osborne AL, Weston-Green K. Effect of cannabidiol on muscarinic neurotransmission in the prefrontal cortex and hippocampus of the poly I:C rat model of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 2019; 94:109640. [CrossRef]
- Rohleder C, Müller JK, Lange B, Leweke FM. Cannabidiol as a potential new type of an antipsychotic. A critical review of the evidence. Front Pharmacol 2016; 7:422. [CrossRef]
- Zuardi AW, Morais SL, Guimaraes FS, Mechoulam R. Antipsychotic effect of cannabidiol. J Clin Psychiatry 1995; 56:485-486.
- Leweke FM, Piomelli D, Pahlisch F, Muhl D, Gerth CW, Hoyer C, Klosterkotter J, Hellmich M, Koethe D. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry 2012; 2:e94. [CrossRef]
- Bhattacharyya S, Wilson R, Appiah-Kusi E, O’Neill A, Brammer M, Perez J, Murray R, Allen P, Bossong MG, McGuire P. Effect of cannabidiol on medial temporal, midbrain, and striatal dysfunction in people at clinical high risk of psychosis: a randomized clinical trial. JAMA Psychiatry 2018; 75:1107-1117.
- Blessing EM, Steenkamp MM, Manzanares J, Marmar CR. Cannabidiol as a Potential Treatment for Anxiety Disorders. Neurotherapeutics 2015; 12:825-836. [CrossRef]
- Zuardi AW, Shirakawa I, Finkelfarb E, Karniol IG. Action of cannabidiol on the anxiety and other effects produced by delta 9-THC in normal subjects. Psychopharmacology (Berl) 1982; 76:245-250. [CrossRef] 288 Dusunen Adam The Journal of Psychiatry and Neurological Sciences 2019;32:283-288
- Zuardi AW, Cosme RA, Graeff FG, Guimaraes FS. Effects of ipsapirone and cannabidiol on human experimental anxiety. J Psychopharmacol 1993; 7(Suppl.1):82-88. [CrossRef]
- Crippa JA de S, Zuardi AW, Garrido GEJ, Wichert-Ana L, Guarnieri R, Ferrari L, Azevedo-Marques PM, Hallak JEC, McGuire PK, Busatto GF. Effects of cannabidiol (CBD) on regional cerebral blood flow. Neuropsychopharmacology 2004; 29:417-426. [CrossRef]
- Crippa JAS, Derenusson GN, Ferrari TB, Wichert-Ana L, Duran FLS, Martin-Santos R, Simoes MV, Bhattacharyya S, Fusar-Poli P, Atakan Z, Santos Filho A, Freitas-Ferrari MC, McGuire PK, Zuardi AW, Busatto GF, Hallak JEC. Neural basis of anxiolytic effects of cannabidiol (CBD) in generalized social anxiety disorder: a preliminary report. J Psychopharmacol 2011; 25:121-130. [CrossRef]
- Das RK, Kamboj SK, Ramadas M, Yogan K, Gupta V, Redman E, Curran HV, Morgan CJA. Cannabidiol enhances consolidation of explicit fear extinction in humans. Psychopharmacology (Berl) 2013; 226:781-792. [CrossRef]
- Hsiao YT, Yi PL, Li CL, Chang FC. Effect of cannabidiol on sleep disruption induced by the repeated combination tests consisting of open field and elevated plus-maze in rats. Neuropharmacology 2012; 62:373-384. [CrossRef]
- Soares V, Campos A. Evidences for the anti-panic actions of cannabidiol. Curr Neuropharmacol 2017; 15:291-299. [CrossRef]
- Linge R, Jimenez-Sanchez L, Campa L, Pilar-Cuellar F, Vidal R, Pazos A, Adell A, Diaz A. Cannabidiol induces rapidacting antidepressant-like effects and enhances cortical 5-HT/ glutamate neurotransmission: role of 5-HT1A receptors. Neuropharmacology 2016; 103:16-26. [CrossRef]
- Shoval G, Shbiro L, Hershkovitz L, Hazut N, Zalsman G, Mechoulam R, Weller A. Prohedonic effect of cannabidiol in a rat model of depression. Neuropsychobiology 2016; 73:123-129.
- Karl T, Garner B, Cheng D. The therapeutic potential of the phytocannabinoid cannabidiol for Alzheimer’s disease. Behav Pharmacol 2017; 28 (2 and 3-Spec Issue):142-160. [CrossRef]
- FDA News Release. FDA approves first drug comprised of an active ingredient derived from marijuana to treat rare, severe forms of epilepsy. https://www.fda.gov/news-events/pressannouncements/fda-approves-first-drug-comprised-activeingredient-derived-marijuana-treat-rare-severe-forms. Accessed August 23, 2019.